65 year old male patient with SOB and chest pain
This is an online E Logbook to discuss our patient's de-identified health data shared after taking his/her guardian's signed informed consent. Here, we discuss our individual patient's problems through a series of inputs from an available global online community of experts to solve those patients' clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
—————————————————————————————————————————————-
65 year old male patient, resident of chitratigudem, suryapet, farmer by occupation came to casuality with chief complaints of
1. Chest pain since 2 hours
2. Shortness of breath since 2 hours
3. Decreased urine output since morning
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptotic 2 hours ago, then developed chest pain and shortness of breath after eating spicy food, having 30 ml of alcohol.
Pain was insidious in onset gradually progressive, non radiating, associated with shortness of breath (grade 3), pain and burning sensation in the stomach.
No complaints of right shoulder pain, sweating , nausea, vomitings
PAST HISTORY:
No similar complaints in the past
K/C/O hypertension since 1 year and is on medication (Atenolol 25mg)
(He met with an accident 1 year ago, then he was diagnosed with HTN)
SURGICAL HISTORY :
Gallbladder stenting was done 5 years ago, and was asked to come back after 2 years for removal but patient never went back due to financial issues
( c/o pain in the right hypochondrium and right iliac fossa for which he went to a private hospital where stenting was done)
Patient met with an accident 1 year go ( bike vs bike) had left lower leg fracture (? Tibia/fibula )
For which intramedullary nail was placed.
Patient also underwent a spinal surgery (disc prolapse of lumbar vertebrae ) 8 months ago
( c/o pain and weakness of both the lower limbs )
Patient stopped going to work after the surgery.
His daily life activities such as squatting, sitting crossed legged have been greatly compromised
He is not even able to sleep in the same position for long hours
PERSONAL HISTORY:
DIET: mixed, contains a lot of spicy food
APPETITE : normal
BOWEL AND BLADDER : regular
SLEEP: adequate
ADDICTIONS :
Alcohol since 30 years : occasionally has 90 ml of whiskey
Smoking since 25 years : smokes 4packs / day
But stopped 5 years ago, just after the stenting surgery
Examination:
Patient is conscious, coherent, cooperative
Well oriented to time/person/place
No pallor/cyanosis /icterus / clubbing / lymphadenopathy
Edema of the both the lower limbs present (right > left)
Vitals :
Afebrile
BP: 130/80mm hg
PR: 84bpm
GRBS: 240 mg/dl
RR: 18cpm
SYSTEMIC EXAMINATION:
CVS: S1S2 +, NO MURMURS
RS: BAE+, CLEAR
P/A: SOFT, NON TENDER, BS+
CNS: NAD
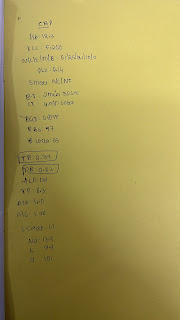
INVESTIGATIONS:
27/04/2022
Hemogram:
Blood group: O positive
HB: 12.1 gm/dl
TLC: 11,900
PLT: 2.41
BT: 2 min
CT: 4min
RBS: 140 mg/dl
Uric acid: 4.7
S.creat: 1.6
Urea: 26
Na: 139
Cl: 102
K: 3.6
LFT:
TB: 0.56
DB: 0.26
SGOT: 23
SGPT: 17
ALP: 130
TP: 6.4
ALB: 3.4
A/G: 1.16
CUE:
ALB: +
SUGAR: NIL
DIAGNOSIS:
Acute gastritis
Treatment given:
1. INJ. Pan 40 mg
2. INJ. ZOFER
3. INJ. Tramadol in 100 ml NS
Advice on discharge :
1.Tab. Pan 40 mg OD X 7 days
2. Syp. SUCRALFATE 10ml TID X 7 days
3. Strict avoidance of Alcohol



Comments
Post a Comment