60 year old female with fever and thrombocytopenia
This is an online E Logbook to discuss our patient's de-identified health data shared after taking his/her guardian's signed informed consent. Here, we discuss our individual patient's problems through a series of inputs from an available global online community of experts to solve those patients' clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
—————————————————————————————————————————————-
A 60 year old female, resident of Peddagudem, Nalgonda, Farmer (in cotton farm) by occupation, came to the casualty with complaints of
- Fever since 6 days associated with chills and rigor.
- Melena since 2 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently normal 6 days back, then she developed fever which was sudden in onset, no diurnal variation, associated with chills and rigor, relieved on medication given by the local doctor. (?Paracetomol + IVF)
2 days later, she started to sweat profusely - for which they sought consultation at outside hospital and was referred here in view of low platelet count and dengue NS1Ag +ve.
At the same time she complained of dark stools (?melena)
No history of SOB/ palpitations/ headache/ cough/ body ache.
PAST HISTORY :
1 year back, she went to the hospital in view of weakness and was diagnosed with hypertension and was on T. Amlodipine 5 mg since then.
Patient is complaining of joint pains since 20 years
Initially started in both the shoulders, then gradually progressed to involved bilateral knees and later to the small joints ( wrist joint)
She consulted local doctor in miryalaguda for the same and started using medications
(? Rheumatoid arthritis)
Patient is also complaining of lower abdominal pain with increased frequency and urgency of urination since 15 days, which was relieved no passing urine
Hysterectomy done 15 years ago due to mass in the uterus (?fibroid)
Not a known case of Diabetes mellitus, TB, CAD, Asthma.
GENERAL EXAMINATION :
Patient is conscious, coherent, cooperative
Well oriented to time and place.
No pallor, icterus, cyanosis, lymphadenopathy, edema.
Vitals -
Temperature : 98.6f
Pulse : 92bpm
Blood pressure : 130/90 mmhg
Respiratory rate : 22 cpm
SYSTEMIC EXAMINATION :
PA : Soft, non tender. No guarding, rigidity. Bowel sounds +
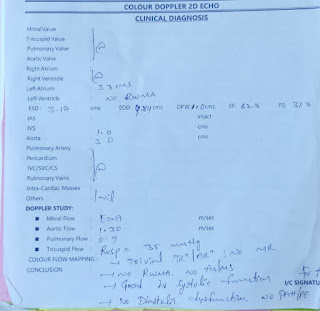
CVS : S1 S2 present, no murmurs.
RS : BAE +, NVBS heard. No crepts.
CNS : NAD
PROVISIONAL DIAGNOSIS :
Fever with thrombocytopenia with NS1Ag +ve
INVESTIGATIONS :
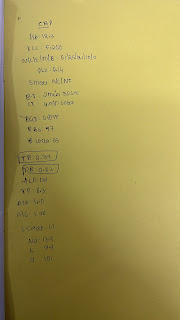
Hemogram -
Hb : 14.6 g/dl
PLT : 22000
WBC : 10880
N : 8080
L : 1150
M : 1440
E : 10
9:30 AM
Hb: 14.6 g/dl
PLT: 30,000
2:00 PM
Hb: 12.5 g/dl
PLT : 60,000
RBS : 260 mg/dl
RFT -
Blood urea : 57 mg/dl
Uris acid : 6.6 mg %
Serum creatinine : 1.2 mg/dl
Sodium : 136 meq/l
potassium : 6 meq/l
Chlorine : 98 meq/l
LFT -
Total bilirubin : 1.09 mg/dl
Direct bilirubin : 0.54 mg/dl
SGOT : 586 IU/dl
SGPT : 292 IU/dl
ALP : 277 IU/dl
Total proteins : 5.9 g/dl
Albumin : 3.4 g/dl
A/G : 1.45
NS1 : +ve
IgM : +ve
IgG : +ve
BGT : A+Ve
RA factor: negative
CRP: negative
ESR: 60 mm/ 1st hour
TREATMENT :
1. IVF - NS, RL at 100 ml/hr
2. INJ. OPTINEURON 1 amp in 100ml NS IV/OD
3. INJ. NEOMOL 1G IV SOS (if temp >101f)
4. INJ PAN 40MG IV/OD
5. INJ ZOFER 4 MG IV/SOS
6. TAB. PCM 500MG PO/TID
7. TAB. AMLODIPINE 5MG PO/OD
8. INJ. THIAMINE 2 amp in 100ml NS IV/OD
Vitals:
Temperature: 98.61F
Bp: 120/90 mm hg
PR: 90 bpm
RR: 20 cpm
SPO2: 98 %
GRBS: 112 mg/dl
SYSTEMIC EXAMINATION:
CVS: S1S2 +
RS: BAE+
P/A: SOFT, NON TENDER
CNS: NAD
A- FEVER WITH THROMBOCYTOPENIA WITH NS1 POSITIVE
P- 1. IVF - NS, RL at 100 ml/hr
2. INJ. OPTINEURON 1 amp in 100ml NS IV/OD
3. INJ. NEOMOL 1G IV SOS (if temp >101f)
4. INJ PAN 40MG IV/OD
5. INJ ZOFER 4 MG IV/SOS
6. TAB. PCM 500MG PO/TID
7. TAB. AMLODIPINE 5MG PO/OD
8. INJ. THIAMINE 2 amp in 100ml NS IV/OD
9. TAB. DOXY 100 MG PO/BD









Comments
Post a Comment