This is an online E Logbook to discuss our patient's de-identified health data shared after taking his/her guardian's signed informed consent. Here, we discuss our individual patient's problems through a series of inputs from an available global online community of experts to solve those patients' clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
—————————————————————————————————————————————-
37 year old female a resident of Dugapally , housewife was brought to the casuality with complaints of
1. Neck pain since 4 days
2. Fever since 4 days
3. Body pains since 4 days
4. Altered sensorium since yesterday
HOPI:
Patient was apparently asymptomatic 4 days back then she had neck pain which was insidious in onset and gradually progressive followed by burning of eyes then developed fever associated with chills and rigors din’t subside on medication
patient’s attender took her to the local RMP for fever and was started on antibiotics.
Patient attender observed altered sensorium since yesterday and was brought to the hospital for further evaluation
N/K/C/O HTN,DM,THYROID,ASTHMA,CAD
Surgical history:
History of tympanoplasty 5 years ago
On presentation:
patient is drowsy arousal to painful stimulus
VITALS
febrile 101.3 F
B.P - 170/90 mm hg
PR- 101 bpm
RR: 18 CPM
SYSTEMIC EXAMINATION
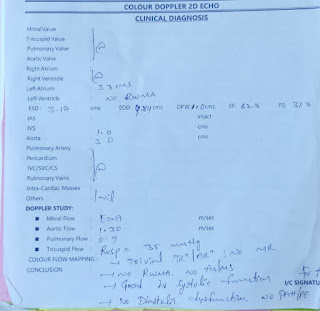
Cvs - s1 s2 heard no murmurs
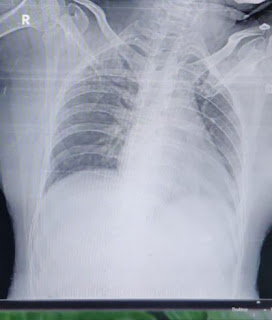
RS :- NVBS no adventitious sounds
Kernig’s sign positive
Brudzinski’s sign positive
Lumbar puncture was performed
INVESTIGATIONS:
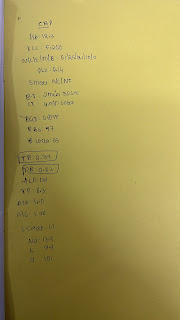
CSF ANALYSIS
TC -112 cells
Dc- predominantly lymphocytes
Rbc’s - Nil
Sugar-38
Protein -102
Chloride-98
BGT: O POSITIVE
APTT: 30 SEC
PT: 15 SEC
INR: 1.11
HEMOGRAM:
HB: 12.9
TLC: 9,400
PLT: 3.39 L
LFT:
TB: 0.77
DB: 0.18
AST: 20
ALT: 35
ALP: 228
TP: 6.6
ALB: 3.7
A/G: 1.32
RFT:
S. Creat: 0.6
Na+ : 134
Cl- : 96
K+ : 3.0
URIC ACID: 1.8
BLOOD UREA: 17
RBS: 141 MG/DL
CUE:
COLOUR: PALE YELLOW, CLEAR
SP GRAVITY: 1.010
NO ALBUMIN/SUGARS/BILE PIGMENTS/BILE SALTS /RBC
PUS CELLS: 3-4
EPITHELIAL CELLS: 2-3
SPOT URINE PROTEIN: 7.5
SPOT URINE CREATININE : 44.2
RATIO: 0.16
DIAGNOSIS :
TUBERCULAR MENINGITIS
TREATMENT :
1. IVF NS and RL @ 75ml/ hour
2. RT FEEDING 2nd hourly- 200ml
3. Tab. RIFAMPICIN 600mg
4. TAB. ISONIAZID 300 mg
5. TAB. PYRAZINAMIDE 1500mg
6. TAB. ETHAMBUTOL 1900 mg
7. INJ. CEFTRIAXONE 2gm/IV/BD
8. INJ. PAN 40 mg /IV/ BD
9. INJ. ZOFER 4mg/ IV/SOS
10. INJ. NEOMOL 100ml (if temp > 101.1F)
11. Head end elevation by 30 degree
12. Vital monitoring hourly
13. Fever charting 4th hourly
SOAP NOTES DAY 1:
S- no fresh complaints
O- patient is drowsy
Sensorium improved
Not oriented to time/place/person
Recalling her name
Neck rigidity +
Kernigs sign +
Brudzinski sign +
Pro did of the left eye lid
Left conjunctival congestion And swelling present
Vitals:
Temp: 99.1 F
BP: 140/100 mmhg
PR: 90bpm
RR : 18cpm
SPO2: 98% on RA
I/O: 2700ml / 1050 ml
Stools: not passed
SYSTEMIC EXAMINATION:
CVS: S1S2 present , no added sounds
RS: BAE+
P/A: soft, non tender
A- TB MENINGITIS
P-
1. IVF NS and RL @ 75ml/ hour
2. RT FEEDING 2nd hourly- 200ml
3. Tab. RIFAMPICIN 600mg
4. TAB. ISONIAZID 300 mg
5. TAB. PYRAZINAMIDE 1500mg
6. TAB. ETHAMBUTOL 1900 mg
7. INJ. CEFTRIAXONE 2gm/IV/BD
8. INJ. PAN 40 mg /IV/ BD
9. INJ. ZOFER 4mg/ IV/SOS
10. INJ. NEOMOL 100ml (if temp > 101.1F)
11. Head end elevation by 30 degree
12. Vital monitoring hourly
13. Fever charting 4th hourly
E1V2M4,BP-160/100mmhg,Pr-80/min before LP at 5:00pm on 23/04/2022
After LP pt GCS-E1V2M4 ,Bp-170/100mmhg,Pr-78/min
Given DEXA 8mg & ceftriaxone 2g x IV x BD
ATT given at 10pm
Pt became conscious at 8:00am on 26/4/2022
GCS-E4V2M4,Opening of right eye, Ptosis of lf eye,Anisochoria(Rt eye-Mid dilated reacting to light,Lf eye-Dilated & sluggish reactive to light),Bp-180/100mmhg,Pr-84/min
At 1pm Pupils Rt eye-Mid dilated non reacting to light & Lf eye Full Dilated non reacting to light
At 5Pm GCS-E4V3M4,Bp-170/100mmhg,Talking of inappropriate words on questioning
At 11:00pm E3V3M4,Bp-180/100mmhg,Pr-70/min
Patient @5a.m ,Had no central and peripheral pulses ,Hr-20/min ,ROSC obtained after 6 cycles of cpr , intubated and connected to mechanical ventilator in acmv-vc mode
and @ 8:10 a.m. patient ‘s central and peripheral pulse was not detected cpr was initiated and 6 cycles of cpr was done and patient could not be revived. The patient was declared dead @ 8:33 a.m. with ecg showing no electrical activity







Comments
Post a Comment