51 year old with COVID PNEUMONIA
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
————————————————————————————————————————————————
An Outline about the Patient :
He is a 51 year old gentleman from a village in South India.
Chief Complaints : The Patient presented on 1/06/2021 with Cough since 6 days , Chest Pain since 4 days
History of Presenting Illness :
The patient was apparently asymptomatic 6 days back when he developed Cough ( wet ) .It was insideous in onset . The expectoration was minimal in amount , mucoid in consistency , non foul smelling , non blood stained . Not aggravated or relieved with posture.
He developed Chest pain 4 days back , sharp in nature , not radiating to back , or upper limb . Pain aggravated on respiration movements of the chest and on coughing as well , no relieving factors as such.
COVID RTPCR done at the hospital on 3/6/21 and positive results obtained.
There is no History of
Shortness of Breath
Hemoptysis
Fever
Body Pains
Fatigue
PAST HISTORY :
History of previous infection with COVID 19 on 13/05/21 , for which he had been hospitalized and was given O2 Support for 5 days before his discharge on the 6th Day.
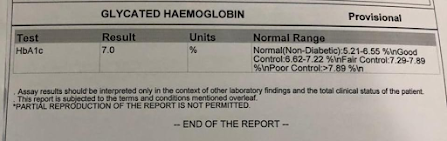
He is a K/C/O DM, ( Since 9 years , takes Glimiperide 2mg , Metformin 500 mg BD )
HTN ( Since 3 years , takes Amlodipine 5 mg O.D )
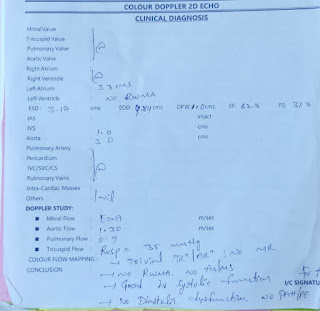
No past H/o CAD , Asthma , Epilepsy .
PERSONAL HISTORY :
He has normal appetite ,
Takes Mixed Diet
Sleep slightly disturbed due to Cough
Constipation since the last 5 days.
Not an alcoholic.
Used to Smoke but stopped 12 years back.
No known Allergies.
Family History :
Contacts being traced for any COVID infected indivual ( if any ).
GENERAL EXAMINATION :
Done after obtaining consent , in a well lit room , in the presence of an attendant , with adequate exposure .
No pallor , Icterus , Cyanosis , Clubbing , Koilonychia , Generalised Lymphadenopathy or Pedal Edema.
Pt c/c/c
Bp: 130/90 mmhg
PR: 96/min
SpO2: 98%
RR: 22/min
Temp: 97.5F
GRBS: 334mg/dl
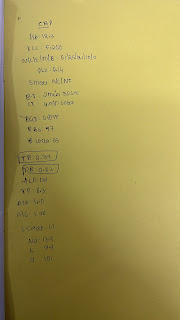
CBP:
Hb: 10.2
TLC : 12,200
PLT: 2.77
5/06/2021
Bp: 120/90 mmhg
PR: 92/min
SpO2: 98%
RR: 22/min
Temp: 97.5F
GRBS: 327mg/dl
6/06/2021
Bp: 120/90 mmhg
PR: 96/min
SpO2: 98%
RR: 20/min
Temp: 97.5F
GRBS: 312mg/dl
RADIOLOGICAL INVESTIGATIONS :
PROVISIONAL DIAGNOSIS :
UPDATE :
7/JUNE/2021
Patient Discharged






















Comments
Post a Comment