CASE OF A 36 YEARS OLD MALE WITH SEVERE VIRAL INTERSTITIAL PNEUMONIA
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
—————————————————————————————————————————————
This is a case of 36 years old male who came to the hospital on 29th May with :
CHIEF COMPLAINTS:
1) Fever since 5 days
2) Cough since 4 days
3) Shortness of breath since 4 days
HISTORY OF PRESENT ILLNESS :
The patient was apparently asymptomatic 5 days back then he developed a fever which was sudden in onset , intermittent in nature, evening rise of temperature associated with chills .
The patient got tested for COVID-19 and the result came out to be positive on 21st May and was self isolated since then.
He developed dry cough 4 days back which was insidious in onset, intermittent in nature with no diurnal or positional variations .
Then he developed shortness of breath 4 days back (grade II) which was insidious in onset and gradually progressive .
Since 2 days the patient started experiencing SOB grade IV ( NYHA ) so he went to an outside hospital for treatment. The HRCT chest report interpreted severe viral interstitial pneumonia with a severity score of 18/25 and CORADS-5. So he was advised to get treated in the present hospital .
He also had body pains and loss of smell and taste .
No complaints of headache, chest pain, diarrhea, cold, sore throat.
PAST HISTORY:
Not a K/C/O Diabetes Mellitus, hypertension, asthma, TB, epilepsy.
PERSONAL HISTORY :
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel and bladder movements: Regular
Addictions: Occasionally drinks alcohol ( 3-4 times in a month , 90ml each time)
No known allergies
FAMILY HISTORY :
The patient's family members including his wife and child all tested positive for COVID-19.
GENERAL EXAMINATION:
The patient was examined in a well lit room with informed consent.
Patient was conscious, coherent and cooperative, well oriented to time, place and person.
- Pallor : Absent
- Icterus: Absent
- Cyanosis: Absent
- Clubbing: Absent
- Lymphadenopathy : Absent
- Edema : Absent
VITALS :
At the time of admission:
- Temperature : Afebrile
- BP -120/80mmhg
- PR- 72/min
- Spo2- 78% on RA
On 31/5/21:
- Temperature - Afebrile
- BP : 120/80 mm/Hg
- PR: 70/min
- SpO2 : 90% on 15L of NRBM
On 1/6/21:
- Temperature : Afebrile
- Pulse rate : 60 cycles/min
- Blood pressure : 120/80 mmHg
- SpO2: 89% on 15L NRBM
SYSTEMIC EXAMINATION :
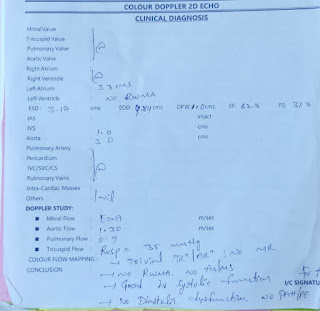
CVS : S1 and S2 heard
No added thrills and murmurs
RS : Normal vesicular breath sounds heard, BAE +
PER ABDOMEN : soft, non-tender
CNS: HMF normal
LAB INVESTIGATIONS :
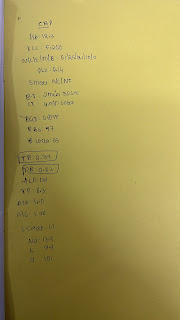
HEMOGRAM :
- Hemoglobin: 14.8
- TLC : 6,400
- PLT: 2.15L
1/6/21
- Hb: 16.4
- TLC: 9,200
- PLT: 2.84
LFT:
- Total Bilirubin - 0.98mg/dl
- Direct Bilirubin - 0.21mg/dl
- AST - 51 IU/L
- ALT - 43 IU/L
- ALP - 177 IU/L
- Total Proteins - 5.7 gm/dl
- Albumin - 3.0 gm/dl
- A/G - 1.14
RFT :
- Urea - 26 mg/dl
- Creatinine -1.0mg/dl
- Uric Acid- 4.2 mg/dl
- Ca+2 - 10.0mg/dl
- PO4 - 3.9 mg/dl
- Na+ - 138 mEq/L
- K+ - 4.1mEq/L
- Cl- 99 mEq/L
LDH : 513
ESR : 60
D.DIMER : 10
CRP : +ve (1.2)
FERRITIN : > 1500
CT SCAN : ( Taken on 29/5/21 )
CORADS : 5
DIAGNOSIS : SARS COVID-19 VIRAL PNEUMONIA
TREATMENT:
1. O2 inhalation to maintain SpO2>92%
2. Intermittent BiPAP if dyspnoea increases
3. INJ. DEXAMETHASONE 6mg IV OD (D4)
4. INJ. CLEXANE 40mg PO OD (D4)
5. TAB. PANTOP 40mg PO OD
6. TAB. MVT PO OD
7. TAB. LIMCEE PO OD
8. TAB. DOLO 650mg PO TID
9. SYP. GRILLINCTUS 2tbsp TID
10. GRBS at 8 am
11. BP /SpO2/ PR/ RR hourly
12. Monitor vitals







Comments
Post a Comment