This is an online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
—————————————————————————————————————————————————-
CASE DISCUSSION
A 85 year old male who is a carpenter by occupation came to the opd with
Chief complaints of SOB since 5 hours
History of present illness:
Patient was apparently asymptomatic one day back and then he developed SOB which was sudden in onset and progressive in nature and present even at rest (Grade 4)
History of fever 5 days back which was high grade associated with chills and rigor
Relieved on taking medication
He complaints of constipation since 2 to 3 months and pass the stool once every 4 to 5 days
He had involuntary micturition on the day of admission at afternoon which was associated with pain
He also had a history of involuntary micturition 2 years ago for which he had been treated by a local RMP
Memory loss since 1year
He tested positive for covid 19 on 3rd June
History of past illness:
A known case of hypertension since 30 years
A known case of dm since 7 years
He was operated for gall bladder stones 10 years ago (cholecystectomy)
Personal history:
Appetite: decreased (since 1 month)
Diet:mixed
Sleep: excessive ( since few days)
Bowel: irregular Passed stools once in 4-5 days
Micturition: abnormal ( involuntary micturition on the day of admission)
No known allergies
Addictions: Stopped alcohol consumption and beedi smoking 15 years ago
Family history: insignificant
Drug history :
Tab Telma for hypertension
Tab Glycomet for DM
Tab Clopitab since 2 years
General physical examination:
The patient was examined in a well lit room
Vitals on admission
Pulse rate: 117 bpm
Blood pressure: 110/80 mmHg
Respiratory rate : 38 cpm
Temperature: 100.1 °F
Vitals on 03-06-2021:
Pulse rate: 95 bpm
Blood pressure: 100/60 mmHg
Temperature: 98.7 °F
SPO2: 98% with 12L of O2
Vitals On 04-06-2021
Systemic examination on 03-06-2021
CVS S1 and S2 heard
No cardiac murmurs
No thrills
Respiratory:
normal vesicular breath sounds present
B/L wheeze present in IAA and ISA (L>R)
Dyspnea is present
B/L crepitus present
Per abdomen:
Shape of abdomen: distended
diffuse tenderness is present
No palpable mass
Hernial orifices are normal
No free fluid present
Liver is not palpable
Spleen not palpable
Bowel sounds are heard
CNS:
Level of consciousness: stuporous
Speech: no response
Signs of meningial irritation present:
Neck stiffness present
Kernings sign is postive
GCS: E2 V1 M4
Tone of muscles : increased in all four limbs
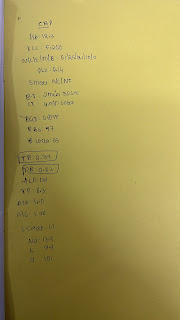
Right Left
Power of muscle
Upper limb. 2/5. 2/5
Lower limb 2/5. 2/5
Reflexes
B T S A K P
Right. 3+ 3+ 3+ 3+ 3+ withdrawal
Left. 3+ 3+ 3+ 3+ 3+ withdrawal
Investigations:
ABG:
Complete blood picture:
Complete urine examination:
Renal function test:
Hyperkalemia ( drug induced? ARB's?)
Liver function test:
ECG
Left lower lobe consolidation present
MRI brain:
Covid 19 pneumonia with AKI ( pre renal cause)
Atypical Parkinsonism-MSA
Treatment:
Day 1:(02-06-2021)
Tab METROGYL 100 ml / 1V / TID
Inj HYDROCORTISONE 100 mg IV stat
Inj TAZAR 4.5 gm IV stat followed by 4.5 gm IV TID
Tab. AZITHROMYCIN 500 mg OD
Day 2:(03-06-2021)
INJ AUGMENTIN 1.2 gm/ IV/BD
INJ PANTOP 40 mg/IV/OD
Nebulization with DUOLIN And BUDECORT 6th hourly
INJ HAI 8 U in 25% Deutrose / IV /stat
Monitor GRBS 6th Hourly
INJ NEOMOL 1gm/IV/SOS (If temp > 101°F)
Tab. PCM 60mg
I/O – CHARTING
Temp Charting 6th Hourly and tepid sponging
IVF 0.9 % NS with 1 ampule optineuron @ 75 ml/ hr
Day 3:(04-06-2021)
Inj -clexane 40 mg s/c OD
Inj Augmentin 1.2gm I/V BD
Inj Pan 40 mg I/V OD
Nebulization with DUOLIN And BUDECORT 6th hourly
Inj Dexa 8 mg I/V OD
Inj. Human Actrapid
Inj. Neomol 100 ml given
Dialysis
Common causes:
1.Intradialytic hypotension
Systolic bp fall by > 20 mmHg within first 30 minutes of dialysis.
2.muscle cramps
3.Nausea and vomiting
4.Fever
Uncommon causes:
1.Dialysis disequilibrium syndrome( increase ICT and Cerebral oedema)
Seen in first dialysis
Prolonged dialysis and Increased ultrafiltration rate.
2.Dialyser reactions:
Type A:
Serious reactions due to ethylene oxide.
Severe chest pain
Cardiac arrest.
Type B:
Seen after 15-30 minutes.
Slight chest discomfort is present
3 Arrhythmias
4.air embolism
5.haemolysis













Comments
Post a Comment